Imagine a life where every new day fades into a mist of forgotten memories and foggy thoughts. For many, this isn’t just a thought exercise but a reality they live with due to the invisible yet relentless effects of prolonged alcohol abuse. Often overshadowed by the immediate physical repercussions of addiction, the long-term cognitive impacts remain an area shrouded in concern and curiosity.
Alcoholic dementia is a condition that subtly erodes the mind’s once-sharp edges. It profoundly changes lives, relationships, and the essence of what makes us who we are. It manifests as a gradual decline in cognitive function, a slipping grip on reality, and a profound transformation of one’s character and abilities.

What is Alcoholic Dementia and How Does it Affect Individuals?
Alcoholic dementia, also known as alcohol-related brain damage, is a form of cognitive decline caused by prolonged excessive alcohol consumption. It affects individuals by impairing memory, problem-solving skills, and emotional regulation.
This condition can lead to significant changes in personality and behavior, impacting an individual’s ability to perform daily tasks and maintain relationships. Early detection and reduction of alcohol intake are crucial for managing its progression.
Why Does Alcoholic Dementia Occur: Understanding the Causes?
Several key factors contribute to the development of Alcoholic Dementia. Here is a list of some of the causes for this progressive disease:
- Neurotoxic Effects of Alcohol: Alcohol can be neurotoxic, meaning it can damage brain cells directly. Chronic exposure to high levels of alcohol disrupts the brain’s delicate chemistry and structure, leading to cognitive decline.
- Nutritional Deficiencies: Heavy drinking often leads to poor nutrition, particularly a deficiency in vitamin B1 (thiamine), which is crucial for brain health. Thiamine deficiency can lead to serious brain disorders like Wernicke-Korsakoff syndrome, which is closely associated with alcoholic dementia.
- Impact on Brain Structure: Research shows that prolonged alcohol abuse can lead to changes in brain structure, including brain shrinkage, particularly in regions responsible for memory, decision making, and behavior control.
- Genetic Susceptibility: Some individuals may have a genetic disposition that makes their brain more vulnerable to the effects of alcohol, leading to a higher risk of developing cognitive issues with prolonged use.
- Alcohol-Induced Mental Health Disorders: Alcohol abuse can exacerbate or contribute to the development of mental health disorders, such as depression or anxiety, which in turn can affect cognitive function.
- Compounding Factors: Other factors, such as age, other substance abuse, head injuries, and overall health, can compound the effects of alcohol on the brain, accelerating the progression of cognitive decline.
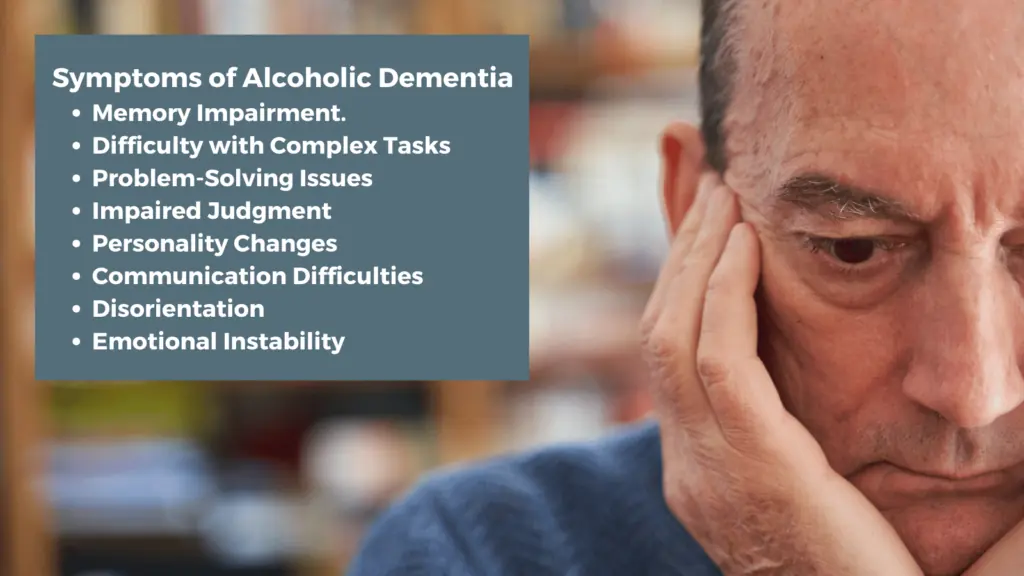
How Can You Recognize the Symptoms of Alcoholic Dementia and Memory Loss?
Recognizing the symptoms of alcoholic dementia is key to early intervention and management. Here are the primary signs to look out for:
- Memory Loss: Individuals may exhibit short-term memory loss, forgetting recent events or conversations. Over time, long-term memory can also be affected.
- Difficulty with Complex Tasks: Those suffering might find it challenging to plan or execute complex tasks that require organization, attention, and management.
- Problem-Solving Issues: There might be a noticeable decline in the ability to solve problems, think abstractly, or understand complex ideas.
- Impaired Judgment: Affected individuals may show poor judgment and decision-making abilities, often resulting in inappropriate social behavior.
- Personality Changes: Look for shifts in personality, such as increased irritability, mood swings, apathy, or a noticeable change in personal habits and hygiene.
- Language and Communication Difficulties: This includes trouble finding the right words, understanding conversations, or engaging in coherent dialogue.
- Disorientation: Individuals may seem lost or confused, even in familiar settings, struggling with time, places, and identifying people.
- Emotional Instability: There may be rapid and unexplained changes in emotions, ranging from aggression to apathy, or inappropriate emotional responses to situations.
What Distinguishes Alcoholic Dementia from Other Types of Dementia?
Distinguishing alcoholic dementia from other types of dementia involves understanding its unique characteristics and impact patterns. Here are key distinctions:
- Cause and Reversibility: Alcoholic dementia, primarily caused by long-term excessive alcohol consumption, often coupled with nutritional deficiencies, is sometimes partially reversible. Reducing alcohol intake and improving nutrition can lead to improvements in cognitive function, unlike many other dementias which are generally progressive and irreversible.
- Pattern of Cognitive Decline: While most dementias, like Alzheimer’s, show a gradual, continuous decline, alcoholic dementia might present a stepwise or fluctuating pattern of cognitive impairment, often directly related to drinking patterns.
- Nutritional Aspect: Alcoholic dementia is often associated with specific nutritional deficiencies, particularly thiamine (Vitamin B1), leading to conditions like Wernicke-Korsakoff syndrome. This link to nutritional aspects is more pronounced in alcoholic dementia compared to other forms of dementia.
- Age of Onset: The onset of alcoholic dementia can vary greatly depending on the individual’s drinking history, but it often affects individuals at a younger age than typical age-related dementia.
- Memory Impairment Nature: In alcoholic dementia, especially in conditions like Wernicke-Korsakoff syndrome, there might be a notable presence of confabulation (fabricating detailed, believable stories to compensate for memory gaps). This is less common in other types of dementia.
- Presence of Liver and Other Physical Health Issues: Due to the nature of alcohol abuse, individuals with alcoholic dementia often have concurrent liver disease or other alcohol-related health issues, which is not necessarily the case with other dementias.
- Brain Structure Changes: Imaging studies often reveal different patterns of brain damage in alcoholic dementia, such as more pronounced shrinkage in specific brain areas related to excessive alcohol use.
What is the Typical Progression of Alcoholic Dementia?
The progression of alcoholic dementia can vary significantly from person to person, influenced by factors like drinking history, overall health, and genetic predispositions. However, a typical progression pattern often includes the following stages:
- 1. Early Stage – Subtle Changes:
- Initially, there might be mild cognitive impairment, noticeable mainly as forgetfulness, slight confusion, or difficulty in solving complex problems.
- Individuals may struggle with tasks that require planning or organization and exhibit poor judgment.
- Changes in mood and behavior, such as increased irritability or apathy, might begin to surface.
- 2. Middle Stage – Increased Impairment:
- Memory problems become more pronounced, especially with short-term memory. The individual might repeat questions or fail to recall recent events.
- Communication difficulties might emerge, including problems with finding the right words or understanding complex sentences.
- There could be noticeable personality changes and a decline in social skills, leading to inappropriate or uncharacteristic behavior.
- Individuals might start experiencing difficulties in daily activities and require assistance with personal care.
- 3. Advanced Stage – Significant Decline:
- Memory loss extends to long-term memories, significantly impacting the individual’s personal identity and history.
- There may be a near-total loss of reasoning and problem-solving abilities, along with severe impairment in judgment.
- Physical health often declines due to the compounded effects of alcohol on various body systems and potential neglect of personal health.
- Complete dependence on caregivers for daily activities becomes necessary as the individual loses the ability to care for themselves.
- 4. Potential for Stabilization or Improvement:
- Unlike many other types of dementia, there’s a potential for stabilization or partial improvement in alcoholic dementia if the individual stops drinking and receives appropriate nutritional support and medical care.
- The degree of recovery can vary widely and is often dependent on the duration and severity of alcohol abuse, as well as the presence of permanent brain damage.
It’s important to note that the progression can be halted or even partially reversed if the individual stops consuming alcohol and addresses nutritional deficiencies, especially in the early stages. However, prolonged and excessive alcohol consumption can lead to permanent brain damage, making some of the cognitive impairments irreversible. Early recognition and intervention are crucial in managing the progression and improving the quality of life for individuals with alcoholic dementia.
How is Alcoholic Dementia Treated: Are There Effective Therapies?
Treating alcoholic dementia involves a multifaceted approach aimed at halting its progression, managing symptoms, and in some cases, reversing cognitive decline. Here are the primary components of treatment:
- Alcohol Abstinence: The most critical step in treating alcoholic dementia is the complete cessation of alcohol intake. This halts further damage and allows the brain to stabilize and potentially recover.
- Nutritional Support: Addressing nutritional deficiencies, particularly thiamine (Vitamin B1), is crucial. High-dose thiamine supplements can be administered, along with a balanced diet to support overall brain and body health.
- Medical Management: Underlying health issues, including liver disease, cardiovascular problems, and other alcohol-related conditions, need to be treated concurrently. Medications may be prescribed to manage symptoms or complications arising from these conditions.
- Cognitive Rehabilitation: Cognitive therapies might be employed to help improve memory, problem-solving skills, and other cognitive functions. This can include memory exercises, problem-solving tasks, and structured activities designed to stimulate cognitive abilities.
- Psychological Support: Counseling or therapy can be beneficial, both for the individual with dementia and their family members. It helps in coping with the emotional and behavioral changes that accompany the condition.
- Social Support: Engaging the individual in social activities and support groups can provide a sense of community and reduce feelings of isolation. Family involvement is also crucial in providing care and emotional support.
- Environmental Adjustments: Creating a safe, structured, and supportive living environment can help manage symptoms and improve quality of life. This might involve modifications to the living space to prevent injuries, establishing routines, and providing supervision or assistance with daily activities.
- Regular Monitoring and Care: Continuous medical evaluation and care are essential to monitor the progression of the disease, manage any emerging health issues, and adjust treatment plans as needed.
While there is no cure for alcoholic dementia, these treatments can significantly improve symptoms, slow down or halt the progression, and in some cases, lead to partial recovery, especially if the condition is identified early and alcohol consumption is completely stopped.
The effectiveness of these therapies varies from person to person, depending on factors such as the extent of the brain damage, overall health, and how quickly treatment is started after the onset of symptoms. A comprehensive approach involving medical, nutritional, psychological, and social interventions offers the best chance for managing the condition and improving the affected individual’s quality of life.

How Can We Help at The Nestled?
Alcoholic dementia is a stark reminder of the profound impact our choices can have on our health and well-being. It underscores the importance of awareness, education, and timely action. But the journey doesn’t end here. For those struggling with alcohol addiction, for families providing care, and for communities seeking to support, there’s a place of solace and a source of strength.
The Nestled, with its commitment to providing resources, guidance, and community support, stands ready to assist those navigating the complexities of alcoholism. Contact us at The Nestled today to find a community that understands and shares your journey. Together, we can face this challenge with knowledge, empathy, and hope.